Studies reveal racial disparities in early US COVID vaccine rollout
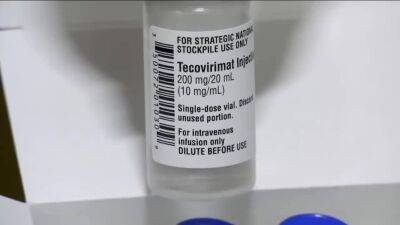
COVID-19 vaccines were less likely to be distributed to US healthcare facilities if they were in counties with a high proportion of Black residents, and racial differences in vaccine uptake may be mainly due to anti-vaccine beliefs among Black adults, according to two new studies highlighting racial disparities in vaccine availability and coverage early in the country's rollout.Role of Black population, urbanicity In the first study, published today in PLOS Medicine, a team led by University of California San Diego researchers studied the availability of COVID-19 vaccines at US healthcare facilities in May 2021.
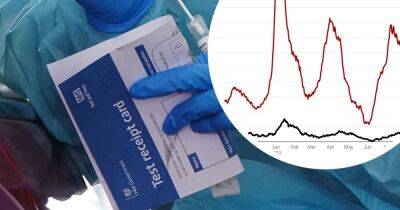
The study included 50,806 community pharmacies, 11,619 federally qualified health centers, 3,187 hospital-based outpatient departments, and 1,255 rural health clinics in 2,942 counties.Nationwide, 61.4% of eligible healthcare facilities and 76.0% of eligible pharmacies provided COVID-19 vaccines.
But facilities in counties in which Black residents made up over 42.2% of the population were less likely to be COVID-19 vaccination sites than those in counties with less than a 12.5% Black population (odds ratio [OR], 0.83; 95% confidence interval [CI], 0.70 to 0.98).Similarly, sites in rural counties (versus metropolitan counties) had lower odds of administrating the vaccines (OR, 0.82; 95% CI, 0.75 to 0.90), as did counties in the top 20% for death rates (OR 0.83; 95% CI, 0.75 to 0.93).Urbanicity and racial composition were significantly linked only in metropolitan counties.
Among these counties, those in which Black residents made up over 42.2% of the population were 32% less likely to administer COVID-19 vaccines than those with less than a 12.5% Black population.Facilities in rural counties with Hispanic
Read more on cidrap.umn.edu